consent_cookie
Duración: 1 year
Stores the user's cookie consent state
03-09-2018
Facing one of the highest HIV prevalence rates in the world, Namibia has become the first country in Africa to have more than three-quarters of its HIV-affected population virally suppressed — and insiders are crediting political commitment, good data, and community-centered HIV programs for the remarkable achievement.
According to the results of Namibia’s first ever population-based HIV survey, known as NamPHIA, the country exceeded many of the 90-90-90 targets set by UNAIDS in 2014. The targets call for countries to get 90 percent of people living with HIV diagnosed; 90 percent of those diagnosed accessing treatment; and 90 percent of people on treatment to have suppressed viral loads by 2020.
Most significantly, 77 percent of people living with HIV in Namibia are now classed as virally suppressed, which means they cannot pass the virus on to someone else. This is higher than the 73 percent target set by UNAIDS — and three years ahead of schedule.
NamPHIA was funded by U.S. President’s Emergency Plan for AIDS Relief PEPFAR as part of a data-drive to support similar population-based surveys in 15 other African countries to reveal gaps in HIV programming.
A new way of testing for HIV
Recent changes to the way HIV testing is done have also helped Namibia reach the U.N. goals. While in the past, undiagnosed HIV patients were generally found by going door to door and testing people, the new approach targets the sexual partners of people newly diagnosed.
Known as index partner testing, the methodology was developed by Centers for Disease Control and Prevention CDC and rolled out in the country starting last year through local NGO DAPP-Namibia, the first high disease burden country to do so.
Ib Hansen, chairman of the Humana People to People network, of which DAPP is a member, said the switch to partner testing had already led to more people being diagnosed and treated. Where under the old method, testers on average found new cases of HIV among 2 percent of people, this figure jumped to 7.7 percent last year with index partner testing, Hansen said. The approach is also credited with reaching a higher number of men than the door-to-door method.
CDC’s Dziuban said the switch was a good example of the ministry of health, and also donor agencies including PEPFAR, being willing to adapt their approach to deliver better results.
“The shift is an example of using data to show where we still have gaps and being willing to shift our programs, and that’s starting at the Ministry of Health level … being willing to adapt and be innovative … and our partners being willing to lead that process of shifting to something that we know will work better for where Namibia is today,’’ he said.
Lela Baughman, PEPFAR country coordinator in Namibia, told that the U.S. funder now wants all of its implementing partners in the country to take up the partner testing approach.
“DAPP has had such great success [in Namibia] with this … so we are now moving all of our implementing partners to the DAPP model,” Baughman said.
DAPP’s personalized and community-based approach to HIV programming
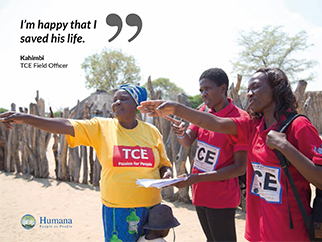
Index partner testing has proved more effective at finding hard-to-reach undiagnosed people in part, because it is more targeted, but also because it is implemented by staff who are embedded in the local community and are able to build relationships, Hansen explained. This is linked to DAPP’s personalized and community-based approach to HIV programming, known as total control of the epidemic, which is designed to systematically reach each person in a community.
DAPP has been implementing this total control of the epidemic in Namibia since 2006, with testing and treatment services led by field offices, which employ local staff and volunteers who develop trusted relationships with the community and those living with HIV. These strong community links make it more likely that people will agree to divulge who their sexual partners are, and that those partners will agree to be tested, Hansen said.
Another element of total control of the epidemic is the “trio system” of support for newly diagnosed people, in which DAPP sets up newly diagnosed HIV patients with a support group of two friends or family members, who are tasked with helping keep the person on ART for the first six months. After that they can join a bigger support group of people undergoing ART treatment, Hansen explained.